- A good SOAP note example shows how to document and communicate patient information.
- A good example SOAP note can help health professionals use a structured format to document patients’ progress during treatment.
- AI note-taking and summarizing technology is revolutionizing healthcare by helping automatically generate effective SOAP notes to avoid burnout.
Anxious about maintaining detailed patient health records? Right. Without detailed and thorough notes, there’s no effective patient care; it’s like working with a heavy heart. Thankfully, a SOAP note example can show you how to keep medical records accurately and completely.
After all, not knowing how to balance medical documentation with patient interaction effectively will weigh heavily on your mind. And that’s where an advanced AI note-taking and transcription tool can come into play to help you effectively structure a standardized format for medical documentation.
Let’s reveal what a SAOP note is, how to craft it correctly using a SOAP note example, and how an AI Assistant can make your note-taking effortless.
What Is a SOAP Note?
Haven’t you heard stories about medical professionals failing to keep accurate health records, thus harming patients’ health? How? They unknowingly repeated an already-done medical procedure that was unallowed.
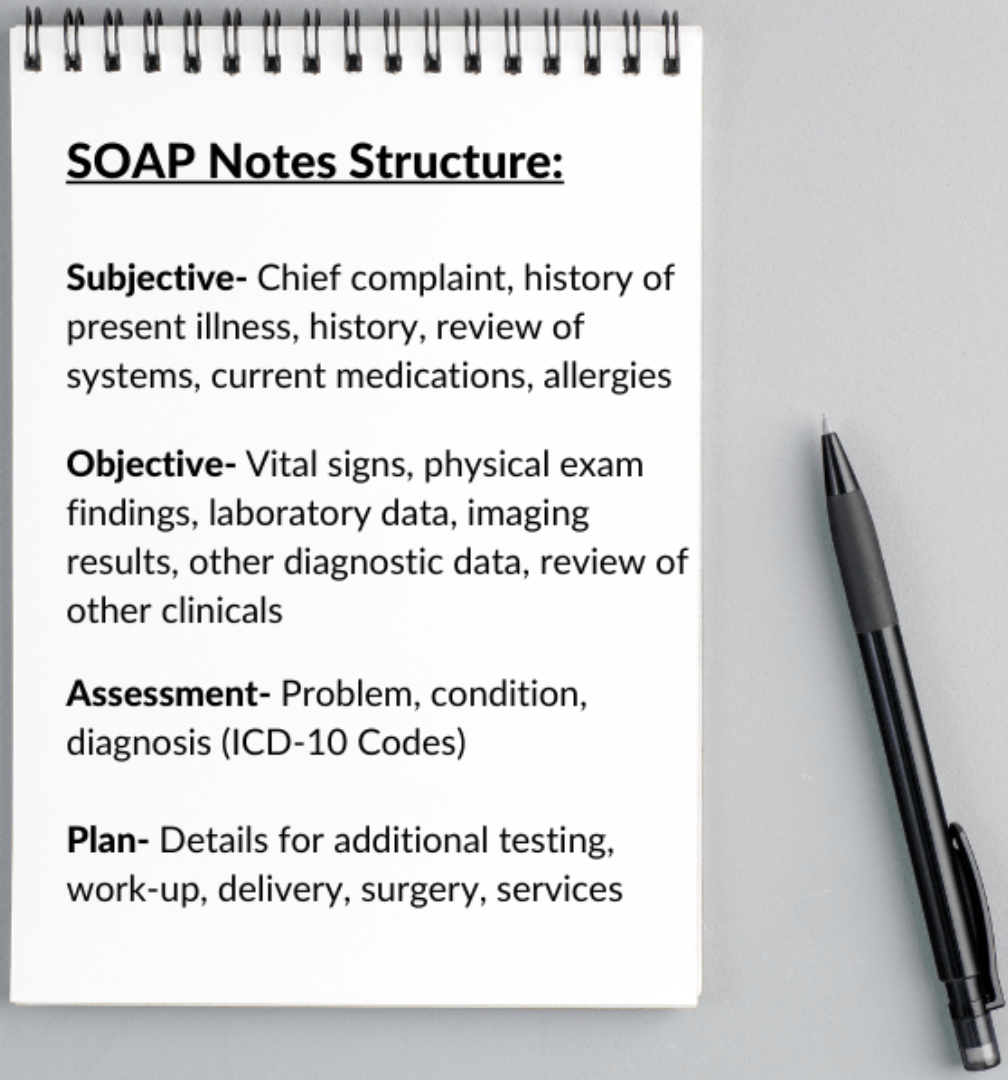
That’s where a SOAP note comes into play. As a documentation method, it helps healthcare providers organize and record patient information accurately and systematically. Why are they called SOAP notes? SOAP means Subjective, Objective, Assessment, and Plan.
A good example SOAP note helps physicians quickly write notes in patients’ charts to make diagnoses, assessments, and decisions. Specifically, these notes include appointment scheduling, patient check-in and check-out, exam, note documentation, rescheduling, mental status exam, assessment, and medical billing.
As a result, communication among medical professionals becomes comprehensive and clear, and Clinical Reasoning and decision-making are facilitated. Clinical Reasoning is the interaction between a therapist and a patient to gather information for optimal diagnosis and treatment.
SOAP notes evolved from the problem-oriented medical records (POMR) developed by Dr. Lawrence Weed in the 1960s. Both methods were epoch-making contributions to healthcare.
What’s the difference between POMR and SOAP records?
- SOAP notes collect the medical record documentation based on the numbered problems on the patient problem list.
- POMR notes organize the documentation based on subjective, objective, assessment, and plan.
What is the difference between a SOAP note and a Progress note?
- SOAP notes have a specific, standardized structure, focus on updates and changes, and organize detailed documentation of patient encounters and assessments.
- Progress notes have a more flexible format and track the patient’s progress and response to treatment over time.
What Is the Structure of a SOAP?
How do you write SOAP notes? A good SOAP note example reflects a structured format for documenting patient encounters in healthcare. It includes four sections to ensure comprehensive, organized, and clear medical records:
- Subjective: Patient-reported symptoms, such as a sharp pain in the lower back and a persistent cough for the past week.
- Objective: Observable and measurable data, such as blood pressure 145/90 mmHg, heart rate 85 bpm, and temperature 100.4°F.
- Assessment: Clinician’s evaluation and diagnosis, such as acute bronchitis and lumbar radiculopathy.
- Plan: Treatment strategy and follow-up, such as “Prescribe ibuprofen for pain, physical therapy referral. Follow up in two weeks to assess pain management and progress.”
How long should a SOAP note be? A good example should be between half a page and one page. The length depends on the complexity of the patient’s condition and visit details. However, the template should be concise and exclude unnecessary information to ensure efficiency in documentation.
What Is the SOAP Note Template?
A SOAP note template wholly and concisely documents the patient’s subjective complaints, objective findings, clinician’s assessment, and treatment plan. Here are samples showing how you can effectively capture the mentioned information to ensure high-quality patient care.
How Do You Write S (Subjective) in SOAP Note?
Record the patient’s reported symptoms, concerns, and history in their own words. Also, add details such as the onset, duration, and symptom intensity. Additionally, include relevant personal or family medical history, lifestyle factors, and current medications.
Here’s a SOAP note example with “S”:
Patient: Jane Doe
Age: 45
Gender: Female
Date: May 29, 2024
Chief Complaint: “I’ve been having severe headaches for the past week.”
History of Present Illness:
Jane reports experiencing throbbing headaches, primarily on the left side of her head, starting about a week ago. The pain is rated 7/10 in intensity and lasts several hours. She mentions that the headaches are worse in the morning and sometimes accompanied by nausea but no vomiting. Jane has tried over-the-counter pain relievers (ibuprofen) with minimal relief.
Associated Symptoms:
- Nausea
- Sensitivity to light and sound
Past Medical History:
- Hypertension (diagnosed five years ago)
- Migraine history (occasional, last occurrence two years ago)
Medications:
- Lisinopril 10 mg daily
- Ibuprofen as needed for headaches
Allergies:
- Penicillin (rash)
Social History:
- Non-smoker
- Occasional alcohol use
- Works as a schoolteacher
Family History:
- Mother has a history of migraines
- Father has hypertension
How Do You Write O (Objective) in SOAP Note?
Capture measurable and observable data. Besides, include vital signs, physical examination findings, and diagnostic test results. Moreover, record specific measurements, such as blood pressure, temperature, and heart rate. Finally, document the information clearly and precisely.
Here’s an example of a SOAP note with “O”:
Vital Signs:
- Blood Pressure: 135/85 mmHg
- Heart Rate: 78 bpm
- Respiratory Rate: 16 breaths per minute
- Temperature: 98.6°F (37°C)
- Oxygen Saturation: 98% on room air
Physical Examination:
- General: Alert and oriented, no acute distress
- Head: Normocephalic, no tenderness on palpation
- Eyes: Pupils Equal, Round, Reactive to Light and Accommodation (PERRLA), no papilledema
- Ears: Tympanic membranes clear, no effusion
- Nose: Nasal passages clear
- Throat: Oropharynx clear, no erythema or exudate
- Neck: Supple, no lymphadenopathy or thyromegaly
- Cardiovascular: Regular rate and rhythm, no mention of murmurs, gallops, or rubs
- Respiratory: Clear to auscultation bilaterally, no wheezes, rales, or rhonchi
- Abdomen: Soft, non-tender, no organomegaly
- Neurological: Cranial nerves II-XII intact, no focal deficits, strength 5/5 in all extremities, DTRs (Deep Tendon Reflexes) 2+ and symmetric, negative Romberg, normal gait.
Diagnostic Tests:
- Complete Blood Count (CBC): WNL (Within Normal Limits)
- Basic Metabolic Panel (BMP): WNL
- MRI of the head: Pending results
How Do You Write A (Assessment) in SOAP Note?
Summarize the patient’s condition based on the subjective and objective data. Additionally, include differential diagnoses and note the significance of the findings. Finally, use clear and concise clinical judgment.
Here’s a SOAP note assessment (A) example:
Chronic Migraine:
Jane presents with a one-week history of throbbing headaches, predominantly on the left side, rated 7/10 in intensity, worsened in the morning, and accompanied by nausea and light sensitivity. She has a history of migraines, last occurring two years ago. The current presentation is consistent with her migraine history.
Hypertension:
Blood pressure today is 135/85 mmHg. Jane has been on Lisinopril 10 mg daily. Her hypertension is currently well-managed but will continue to be monitored.
Nausea:
It is likely associated with migraine episodes. No vomiting was reported.
Pending:
Awaiting MRI results to rule out any intracranial pathology, given the severity and recent onset of symptoms.
How Do You Write P (Plan) in SOAP Note?
Outline the next steps for patient care. Moreover, add prescribed treatments, medications, further diagnostic tests, referrals to specialists, and follow-up appointments. Also, have a specific and actionable plan tailored to the patient’s condition that’ll address all identified issues and concerns.
What is an example of a SOAP note with “P”?
- Chronic Migraine:
Medications:
- Initiate Sumatriptan 50 mg at the onset of headache; may repeat in 2 hours if needed, without exceeding 200 mg in 24 hours.
- Continue the current regimen of Lisinopril 10 mg daily.
Lifestyle Modifications:
- Advise the patient to maintain a headache diary to track triggers, frequency, and intensity.
- Recommend regular sleep schedule, adequate hydration, and avoidance of known migraine triggers (e.g., caffeine, certain foods).
Follow-Up:
- Schedule a follow-up appointment in 4 weeks to assess the effectiveness of the new medication and overall symptom management.
2. Nausea:
Medications:
- Prescribe Ondansetron 4 mg, and take as needed for nausea.
Patient Education:
- Educate the patient on taking Ondansetron only when nausea is severe.
3. Pending MRI Results:
Follow-Up:
- Contact the patient with MRI results once available to discuss further necessary interventions.
Next Steps:
- If MRI is abnormal, consider referral to a neurologist for further evaluation and management.
4. Hypertension:
Management:
- Continue current Lisinopril 10 mg daily.
- Encourage blood pressure monitoring at home and maintain a log for review at the next appointment.
Follow-Up:
- Review the blood pressure log and adjust treatment, if necessary, at the next visit.
Krisp Makes SOAP Note Example Writing Productive
When managing paperwork, physicians feel like overwhelmed clerks drowning in paperwork. Instead of focusing on patient care, they spend significant time on computers, typing away. For example, nurses spend nearly 60% of their time on clinical documentation, according to News Medical.
Such burden leads to considerable stress and burnout, reduced job satisfaction, and poor patient outcomes. The good news is that AI outperforms doctors in summarizing health records wholly and correctly, as research shows.
Krisp, an AI Assistant for note-taking, transcribing, and summarizing, helps craft a perfect SOAP note example to analyze patient data effectively. As clinical innovation officer Jason Hill says, “AI can help humans read messages more closely by highlighting essential pieces of information that are important for the doctor to review.” And, yes, Krisp does this.
How Krisp Contributes to Crafting Your SOAP Notes
President of Mayo Clinic Platform John Halamka says, “Reducing the documentation burden would be a huge win on its own.”
How can Krisp AI Meeting Manager help medical professionals avoid burnout that eventually prompts many to leave?
- Records Doctor-Patient Online Interactions: Krisp records online interactions in real time and with the highest quality. It’s compatible with any virtual conferencing service or platform. Whether you need note taking in Google Meets, Zoom or Teams meetings, the recorded interactions become accessible, actionable resources, boosting productivity and collaboration.
- Distraction-Free Interactions: Krisp’s flagship Noise Cancellation technology has been deployed on over 200M+ devices, processing 80B+ minutes of conversations. Krisp cancels noise, voice, and echo in real time, thus boosting the quality of life.
- Automates Note-Taking, Transcription, and Summaries: Krisp automatically transcribes and summarizes doctor-patient online interactions with exceptional accuracy (96%). These real-time and multilingual transcriptions let you focus on what matters most instead of taking notes.
- Organize Doctor-Patient Interactions into Templates: Krisp provides accurate notes. You can make little edits, remove unnecessary elements, and turn them into a SOAP note example with all relevant details included.
- Eliminates Burnouts and Improves Patient Care: Krisp automates your routine note-taking online to free up your time. As a result, you can spend more time with patients and less time on time-consuming documentation.
- Supports Clinical Decisions: Krisp facilitates your clinical decisions, eliminating manual research. How? It keeps your online interactions recorded with crystal-clear audio so you can revisit and share them with your colleagues for a second opinion.
Additionally, by automating note-taking, Krisp lets you take advantage of every detail and focus on what matters most. Thus, you can make a quality diagnosis and an informed clinical decision.
Finally, you can gather all the clinical information in your detailed, correct, concise SOAP note example for future reference.
Best Practices for Writing Perfect SOAP Notes
With an effective and efficient SOAP note example based on best practices, you can improve patient care and reduce the administrative burden on your shoulders.
- Be Comprehensive: You can have only two sentences per section, and that’s great if they’re easy to comprehend. Compared, you can have five or more sentences in each section without covering what’s needed.
- Include Only the Information that Supports the Patient’s Diagnosis: Write thoroughly yet concisely and precisely. Specifically, add only relevant information concerning the patient and your treatment and approach.
- Write the Way Patients Speak: Describe patients’ pain points using their words. Thus, your SOAP note will accurately reflect their experience. Also, it’ll ensure clarity and help capture their experience authentically.
- Be Objective: Include measurable data, such as diagnostic tests, lab results, and physical exam findings, to have a solid foundation for your assessment. Add results based on actual proof.
- Be Consistent: With a SOAP note example based on a consistent format, you can facilitate reading and finding information quickly.
- Be Accurate and Detail-Oriented: Verify facts and review notes for completeness and consistency before finalizing. Because clear and precise documentation supports effective patient care.
- Leverage AI Tools: For example, AI Assistant Krisp helps transcribe, summarize, and take notes during online patient interactions. Thus, you can streamline the documentation process, save valuable time, avoid errors, and spend more time with patients. And your perfect SOAP note example is ready.
- Outline the Next Steps: Add what treatment should be applied next. Include follow-up and additional tests or referrals.
- Never Delay Documentation: Write timely notes right after communicating with your patient. Thus, you’ll have a complete and accurate image of the condition.
- Double-check: Review and edit your final draft to avoid errors and ensure the information flows logically.
- Comply with HIPPA: Ensure compliance with the US Health Insurance Portability and Accountability Act (HIPPA), legislation ensuring data privacy and security provisions to safeguard medical information.
Wrapping Up
The SOAP note is a widely used documentation format that helps objectively organize and communicate patient health-related findings. The right SOAP note example consists of Subjective, Objective, Assessment, and Plan sections, facilitating effective patient care coordination.
By following best practices, you can create practical and efficient SOAP notes. Importantly, you can enjoy efficiency, accuracy, and time management by integrating AI into crafting SOAP notes.
Moreover, you can significantly reduce physician burnout. And, AI Assistant Krisp, which transcribes and summarizes online interactions, can streamline the creation of comprehensive SOAP notes.
Frequently Asked Questions